Even Higher Concentration Olopatadine (Pataday (TM))
A newer higher concentration (0.77%) version of topical olopatadine is investigated vs. legacy versions of lower concentrations (0.2% and 0.1%) of olopatadine. Ocular itch was reduced for the higher concentration.
Currently, most drugs are marketed as lasting up to 16 hours. By increasing the bioavailability of olopatadine, the new version of this drug could extend to 24 hours (the original marketting for Pata-DAY was supposed to imply once a DAY efficacy) .
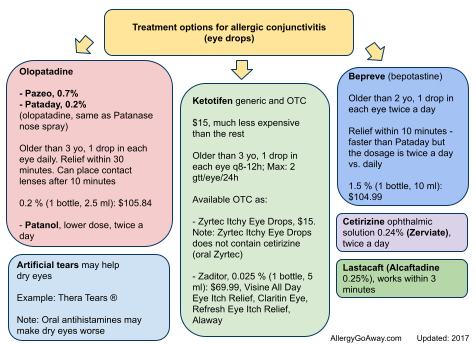
Treatment options for allergic conjunctivitis (eye drops) (click here to enlarge the image).
Cetirizine eye drops
Zyrtec Itchy Eye Drops currently available on the US market actually do not contain Zyrtec (cetirizine), they contain ketotifen. This could change in the future. Cetirizine is a popular over-the-counter oral antihistamine that had already been assessed for a potential ocular allergy treatment in the past. As an oral agent, it may induce dry eyes.
Ophthalmic cetirizine (0.24%) significantly reduced ocular itch up to 8 hours. The drying effect of antihistamines is a conundrum. For nasal sprays, drying effects are highly desirable. For the ocular surface, drying effects can cause havoc. Tear volume can have the effect of increasing the concentration of inflammatory mediators on the eye. With artificial tears, an opposite effect can be seen: increased volume of tears dilute the inflammatory mediators.
Third-Generation H1 and H4 Antihistamines
The H1 receptor was first described more than 40 years ago. The most recently discovered histamine receptor, the H4 receptor, was found in 1994. Current topical antihistamine therapy for allergic conjunctivitis still focuses on H1 receptors. The addition of H4 receptor antagonism may increase efficacy and reduce dosing intervals.
Dry eyes reported more commonly than watery eyes
In Australian Ocular Allergy Study, patients had more frequent symptoms of dry eyes (61%–74%) and itchy or burning eyes (50%–59%) than red eyes, watery eyes, or swollen/puffy eyes.
Artificial tears increase volume of tears and dilute the inflammatory mediators, thus bringing relief of symptoms.
If the comorbidity of allergic conjunctivitis and dry eyes is so high, should an allergist be treating dry eyes?
Treatment options for dry eyes:
1. artificial tears, if not better, add:
2. topical cyclosporine, if not better, add:
3. topical corticosteroid - intraocular pressure must be monitored
References:
Allergy and immunology interfaces with ophthalmology and optometry - Annals of Allergy, Asthma & Immunology, 2014 http://buff.ly/1D6SR1v
A newer higher concentration (0.77%) version of topical olopatadine is investigated vs. legacy versions of lower concentrations (0.2% and 0.1%) of olopatadine. Ocular itch was reduced for the higher concentration.
Currently, most drugs are marketed as lasting up to 16 hours. By increasing the bioavailability of olopatadine, the new version of this drug could extend to 24 hours (the original marketting for Pata-DAY was supposed to imply once a DAY efficacy) .
Treatment options for allergic conjunctivitis (eye drops) (click here to enlarge the image).
Cetirizine eye drops
Zyrtec Itchy Eye Drops currently available on the US market actually do not contain Zyrtec (cetirizine), they contain ketotifen. This could change in the future. Cetirizine is a popular over-the-counter oral antihistamine that had already been assessed for a potential ocular allergy treatment in the past. As an oral agent, it may induce dry eyes.
Ophthalmic cetirizine (0.24%) significantly reduced ocular itch up to 8 hours. The drying effect of antihistamines is a conundrum. For nasal sprays, drying effects are highly desirable. For the ocular surface, drying effects can cause havoc. Tear volume can have the effect of increasing the concentration of inflammatory mediators on the eye. With artificial tears, an opposite effect can be seen: increased volume of tears dilute the inflammatory mediators.
Third-Generation H1 and H4 Antihistamines
The H1 receptor was first described more than 40 years ago. The most recently discovered histamine receptor, the H4 receptor, was found in 1994. Current topical antihistamine therapy for allergic conjunctivitis still focuses on H1 receptors. The addition of H4 receptor antagonism may increase efficacy and reduce dosing intervals.
Dry eyes reported more commonly than watery eyes
In Australian Ocular Allergy Study, patients had more frequent symptoms of dry eyes (61%–74%) and itchy or burning eyes (50%–59%) than red eyes, watery eyes, or swollen/puffy eyes.
Artificial tears increase volume of tears and dilute the inflammatory mediators, thus bringing relief of symptoms.
If the comorbidity of allergic conjunctivitis and dry eyes is so high, should an allergist be treating dry eyes?
Treatment options for dry eyes:
1. artificial tears, if not better, add:
2. topical cyclosporine, if not better, add:
3. topical corticosteroid - intraocular pressure must be monitored
References:
Allergy and immunology interfaces with ophthalmology and optometry - Annals of Allergy, Asthma & Immunology, 2014 http://buff.ly/1D6SR1v