To improve the safety and attractiveness of SIT for patients, alternative routes of allergen administration are being explored:
- sublingual (SLIT)
- oral
The present study (done in mice, not humans) evaluated direct intralymphatic allergen administration with bee venom and cat fur allergens.
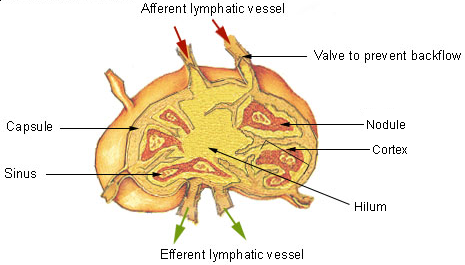
A lymph node showing afferent and efferent lymphatic vessels. Image source: Wikipedia, public domain.
Direct injection of the major bee venom allergen phospholipase A(2) or the major cat fur allergen Fel d 1 into inguinal lymph nodes were compared with subcutaneous injections.
Only intralymphatic immunisation stimulated the production of the Th1-dependent subclass IgG2a, which is associated with improved protection against allergen-induced anaphylaxis.
The authors concluded that in this mouse model, intralymphatic immunisation induced more than 10-fold higher IgG2a responses with 100-fold lower allergen doses than subcutaneous immunisation.
References:
Intralymphatic Injections as a New Administration Route for Allergen-Specific Immunotherapy. Martínez-Gómez JM, Johansen P, Erdmann I, Senti G, Crameri R, Kündig TM. Int Arch Allergy Immunol. 2009 Apr 2;150(1):59-65. [Epub ahead of print]
No comments:
Post a Comment