Dr. Sicherer discussed important papers from the JACI-In Practice on food allergies and anaphylaxis. March 2019 issue will be food allergy centric.
Food allergy themed issue 2018: https://twitter.com/MatthewBowdish/status/1087887030216884225
Wasserman et al on Real World Experience with Peanut OIT: https://twitter.com/MatthewBowdish/status/1087887615972409344
Goals of families doing OIT - 62% wanted to reduce risk of fatal reaction, most thought the risk of death was 1:1,000 to 1:10,000, when data actually suggests risk is 1 in 325,000 over 10 years. An increased threshold from 100 mg to 300 mg peanut in OIT reduces the risk of a reaction by 95%.
Survey for undergoing OIT - motivations include reduce risk of fatal reaction, reduce hassle of avoidance, decrease risks of reaction. This was greater than desire to incorporate foods into diet. QOL: improved after completion of OIT. Low dose OFC to 1.5 mg of peanut likely would allow patients to not worry about precautionary labeling.
Avoidance of peanut precautionary labeling carries individual burdens and costs ($182M per death prevented) - Shaker and Greenhawt.
Baked Potpourri: https://twitter.com/MatthewBowdish/status/1087890228646297600
Baked milk challenges: passing occurs in pts who are younger, with lower IgE. About 70% pass. SPT was not reflective of outcome. If sIGE to milk is less than 8, patients are more likely to pass. They can have serious reactions, more respiratory reactions. Egg allergy leads to more GI reactions.
Dupixent may lead to passing OFCs to foods that were previously not tolerated. Dupilumab and Food Allergy: https://twitter.com/MatthewBowdish/status/1087890535186980864
Any food allergy is a risk factor for asthma with a relative risk of 1.7 to 2.9 depending on specifics.
If you get anaphylactic reactions after VIT, rule out a mast cell disorder, including full workup, beyond just tryptase. Need for lifelong treatment of VIT. Study of 19 patients with severe sting reaction post stopping Venom IT, 18 had clonal mast cell disease, 8 had normal tryptase. Contrary to popular belief, you can get an increase in tryptase during food anaphylaxis, but it's usually 25% rise from baseline rather than over the cut-off of 11ng/ml.
Tryptase and food anaphylaxis: tryptase rose above baseline in 60% of pts. Median rise of 25%. Rise related to severity. Peak is at 2 hrs.
Beta blockers do not seem to block Epi effects in anaphylaxis.
EIA: omega 5 gliadin IgE testing can be helpful in diagnosis. It’s the best predictor of reactivity. You can do an exercise challenges with the suspecting food. You can also do a higher dose food challenge at rest. Cofactors can be exercise and alcohol. sIgE to wheat can be negative.
EoE is prevalent in milk allergic patients. 40% had EoE. 30% were asymptomatic. Risk of EoE in Cow's Milk Allergy: https://twitter.com/MatthewBowdish/status/1087895197705416704
EoE: lots of comorbidities: allergies, immune disorders. EoE Potpourri: https://twitter.com/MatthewBowdish/status/1087895731279560704
EoE: it is rare to outgrow food sensitivity triggering EoE. It occurred only in 9/1,812 patients. EoE was linked to OAS and it improved after removing raw birch-related foods, some patients developed IgE allergies after avoiding foods for EoE. It’s complicated!
Antihistamine allergies: case report to Benadryl, rare event!! But possible. Two papers of allergy/anaphylaxis to antihistamines. It's a rare but it can occur.
There are no detectable food proteins in any common childhood vaccines.
Fructose induced anaphylaxis reported after drinking Coca Cola. Super rare.
FPIES to peanut - there are growing cases with the early introduction following the LEAP study.
There are reported cases of delayed anaphylaxis to shellfish.
Sometimes you need to duplicate SPT, since there can be significant variability, especially when making clinically important decisions.
Milk allergic patients: if they’re severe, 10% can also be allergic to beef and lamb. Especially with undercooked beef. You can do OFCs with well cooked beef. They likely should avoid undercooked meat.
Studies suggest that 26-41% of those with cold-induced urticaria experience systemic reactions, consider epinephrine auto-injector.
---
Mastering Food Allergy Diagnosis
Scott Sicherer presented on "Mastering Food Allergy Diagnosis".
Recommended Food Allergy Testing: history, physical exam, skin prick test, allergen specific serum IgE, elimination diet, oral food challenge. Have to get a good history before ordering tests, don't test foods that are clearly tolerated.
Not recommended food allergy testing: atopy patch test, intradermal test, "combination of tests," unproven tests (IgG, kinesiology, VEGA, etc).
IgE levels in isolation are difficult to interpret. For example, wheat sIGE tends to run high, even sometimes higher than 100, in patients that tolerate wheat, while cashew sIgE tends to run low and you might be worried about low positive levels. 5% of patients with peanut allergies cross react to legumes. Cow milk allergy cross reacts with goat milk in 92%.
What are the challenges to food allergy diagnosis: chronic symptoms, multiple possible triggers, definite outcomes needed, masqueraders (eg Frey's Syndrome), imperfect tests. Dr Sicherer presented a case of Blepharochalasis masquerading as food allergy.
Frey's Syndrome is a rare neurological disorder (fewer than 20,000 cases in US) that may result from injury or surgery near the parotid glands (which manufacture saliva), damaging the facial nerve. Sx: Sweating and flushing of a patch of skin near the ear that occurs when someone is eating.
Different pathophysiologies for different adverse food reactions: https://twitter.com/MatthewBowdish/status/1087427684332761088’
Epidemiology - Child with peanut allergy who has not eaten tree nuts has a 35% risk of tree nut allergy.
Epidemiology - Sibling of child with peanut allergy who has not eaten peanut has 7% risk of peanut allergy.
Child who has atopic derm has 35% risk of having a food involved if eczema is moderate to severe.
10% of patients with milk allergy are also allergic to beef, especially if undercooked.
Sesame seeds don’t have a lot of protein. Sesame allergic patients can tolerate sesame seeds and still be allergic to sesame, so be careful.
Predictive values but must be taken with grain of salt (at arrow): https://twitter.com/MatthewBowdish/status/1087429515935080449
Component testing with risk: https://twitter.com/MatthewBowdish/status/1087431062660177920
Asamoj JACI 2012 130(2):469-72. Shows isolated Ara h8 patients - 144 Swedish pts, 143 passed OFC, 10% had oral symptoms even to cooked peanut but no systemic rxn.
Those with egg IgE less than 2kU/l likely to do well with baked egg challenge. Those with egg sIgE higher than 10kU/L not likely to do well with baked egg challenge. Those with milk IgE less than 5kU/l likely to do well with baked milk challenge. Those with milk sIgE higher than 35 kU/L not likely to do well with baked milk challenge.
Future food allergy diagnostics and prognostics: Basophil activation, ratios (specific IgE to total IgE), epitopes, more components, calculators, DNA methylation patterns.
Food specific IgE to Total IgE: https://twitter.com/MatthewBowdish/status/1087436815206821888
http://cofargroup.org has a predictive calculator for outgrowing egg and milk allergy.
This is a Twitter summary from the 2019 WSAAI meeting. This summary was compiled from the tweets posted by Matthew Bowdish @MatthewBowdish and Ray Firszt @RayFirszt, who attended the 2019 Western Society of Allergy, Asthma and Immunology (WSAAI) meeting. The tweets were labeled #WSAAI. The text was edited by me.
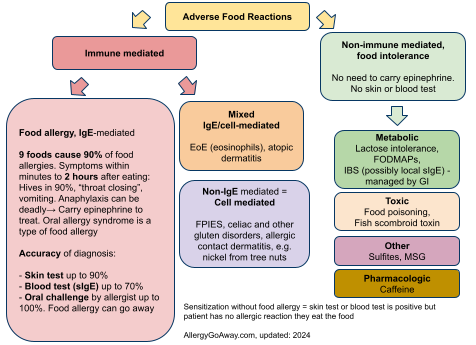
Adverse Food Reactions (click to enlarge the image).
Food allergy themed issue 2018: https://twitter.com/MatthewBowdish/status/1087887030216884225
Wasserman et al on Real World Experience with Peanut OIT: https://twitter.com/MatthewBowdish/status/1087887615972409344
Goals of families doing OIT - 62% wanted to reduce risk of fatal reaction, most thought the risk of death was 1:1,000 to 1:10,000, when data actually suggests risk is 1 in 325,000 over 10 years. An increased threshold from 100 mg to 300 mg peanut in OIT reduces the risk of a reaction by 95%.
Survey for undergoing OIT - motivations include reduce risk of fatal reaction, reduce hassle of avoidance, decrease risks of reaction. This was greater than desire to incorporate foods into diet. QOL: improved after completion of OIT. Low dose OFC to 1.5 mg of peanut likely would allow patients to not worry about precautionary labeling.
Avoidance of peanut precautionary labeling carries individual burdens and costs ($182M per death prevented) - Shaker and Greenhawt.
Baked Potpourri: https://twitter.com/MatthewBowdish/status/1087890228646297600
Baked milk challenges: passing occurs in pts who are younger, with lower IgE. About 70% pass. SPT was not reflective of outcome. If sIGE to milk is less than 8, patients are more likely to pass. They can have serious reactions, more respiratory reactions. Egg allergy leads to more GI reactions.
Dupixent may lead to passing OFCs to foods that were previously not tolerated. Dupilumab and Food Allergy: https://twitter.com/MatthewBowdish/status/1087890535186980864
Any food allergy is a risk factor for asthma with a relative risk of 1.7 to 2.9 depending on specifics.
If you get anaphylactic reactions after VIT, rule out a mast cell disorder, including full workup, beyond just tryptase. Need for lifelong treatment of VIT. Study of 19 patients with severe sting reaction post stopping Venom IT, 18 had clonal mast cell disease, 8 had normal tryptase. Contrary to popular belief, you can get an increase in tryptase during food anaphylaxis, but it's usually 25% rise from baseline rather than over the cut-off of 11ng/ml.
Tryptase and food anaphylaxis: tryptase rose above baseline in 60% of pts. Median rise of 25%. Rise related to severity. Peak is at 2 hrs.
Beta blockers do not seem to block Epi effects in anaphylaxis.
EIA: omega 5 gliadin IgE testing can be helpful in diagnosis. It’s the best predictor of reactivity. You can do an exercise challenges with the suspecting food. You can also do a higher dose food challenge at rest. Cofactors can be exercise and alcohol. sIgE to wheat can be negative.
EoE is prevalent in milk allergic patients. 40% had EoE. 30% were asymptomatic. Risk of EoE in Cow's Milk Allergy: https://twitter.com/MatthewBowdish/status/1087895197705416704
EoE: lots of comorbidities: allergies, immune disorders. EoE Potpourri: https://twitter.com/MatthewBowdish/status/1087895731279560704
EoE: it is rare to outgrow food sensitivity triggering EoE. It occurred only in 9/1,812 patients. EoE was linked to OAS and it improved after removing raw birch-related foods, some patients developed IgE allergies after avoiding foods for EoE. It’s complicated!
Antihistamine allergies: case report to Benadryl, rare event!! But possible. Two papers of allergy/anaphylaxis to antihistamines. It's a rare but it can occur.
There are no detectable food proteins in any common childhood vaccines.
Fructose induced anaphylaxis reported after drinking Coca Cola. Super rare.
FPIES to peanut - there are growing cases with the early introduction following the LEAP study.
There are reported cases of delayed anaphylaxis to shellfish.
Sometimes you need to duplicate SPT, since there can be significant variability, especially when making clinically important decisions.
Milk allergic patients: if they’re severe, 10% can also be allergic to beef and lamb. Especially with undercooked beef. You can do OFCs with well cooked beef. They likely should avoid undercooked meat.
Studies suggest that 26-41% of those with cold-induced urticaria experience systemic reactions, consider epinephrine auto-injector.
---
Mastering Food Allergy Diagnosis
Scott Sicherer presented on "Mastering Food Allergy Diagnosis".
Recommended Food Allergy Testing: history, physical exam, skin prick test, allergen specific serum IgE, elimination diet, oral food challenge. Have to get a good history before ordering tests, don't test foods that are clearly tolerated.
Not recommended food allergy testing: atopy patch test, intradermal test, "combination of tests," unproven tests (IgG, kinesiology, VEGA, etc).
IgE levels in isolation are difficult to interpret. For example, wheat sIGE tends to run high, even sometimes higher than 100, in patients that tolerate wheat, while cashew sIgE tends to run low and you might be worried about low positive levels. 5% of patients with peanut allergies cross react to legumes. Cow milk allergy cross reacts with goat milk in 92%.
What are the challenges to food allergy diagnosis: chronic symptoms, multiple possible triggers, definite outcomes needed, masqueraders (eg Frey's Syndrome), imperfect tests. Dr Sicherer presented a case of Blepharochalasis masquerading as food allergy.
Frey's Syndrome is a rare neurological disorder (fewer than 20,000 cases in US) that may result from injury or surgery near the parotid glands (which manufacture saliva), damaging the facial nerve. Sx: Sweating and flushing of a patch of skin near the ear that occurs when someone is eating.
Different pathophysiologies for different adverse food reactions: https://twitter.com/MatthewBowdish/status/1087427684332761088’
Epidemiology - Child with peanut allergy who has not eaten tree nuts has a 35% risk of tree nut allergy.
Epidemiology - Sibling of child with peanut allergy who has not eaten peanut has 7% risk of peanut allergy.
Child who has atopic derm has 35% risk of having a food involved if eczema is moderate to severe.
10% of patients with milk allergy are also allergic to beef, especially if undercooked.
Sesame seeds don’t have a lot of protein. Sesame allergic patients can tolerate sesame seeds and still be allergic to sesame, so be careful.
Predictive values but must be taken with grain of salt (at arrow): https://twitter.com/MatthewBowdish/status/1087429515935080449
Component testing with risk: https://twitter.com/MatthewBowdish/status/1087431062660177920
Asamoj JACI 2012 130(2):469-72. Shows isolated Ara h8 patients - 144 Swedish pts, 143 passed OFC, 10% had oral symptoms even to cooked peanut but no systemic rxn.
Those with egg IgE less than 2kU/l likely to do well with baked egg challenge. Those with egg sIgE higher than 10kU/L not likely to do well with baked egg challenge. Those with milk IgE less than 5kU/l likely to do well with baked milk challenge. Those with milk sIgE higher than 35 kU/L not likely to do well with baked milk challenge.
Future food allergy diagnostics and prognostics: Basophil activation, ratios (specific IgE to total IgE), epitopes, more components, calculators, DNA methylation patterns.
Food specific IgE to Total IgE: https://twitter.com/MatthewBowdish/status/1087436815206821888
http://cofargroup.org has a predictive calculator for outgrowing egg and milk allergy.
This is a Twitter summary from the 2019 WSAAI meeting. This summary was compiled from the tweets posted by Matthew Bowdish @MatthewBowdish and Ray Firszt @RayFirszt, who attended the 2019 Western Society of Allergy, Asthma and Immunology (WSAAI) meeting. The tweets were labeled #WSAAI. The text was edited by me.
Adverse Food Reactions (click to enlarge the image).