What have we learned from aspirin desensitization in AERD? Twitter summary from the 2019 WSAAI meeting
Katherine Woessner presented on "What have we learned from aspirin desensitization in AERD: How can the methods be improved."
AERD is chronic eosinophilic (Type 2) inflammation of sinuses +/- the lungs with sensitivity to all COX-1 inhibiting NSAIDS with age of onset in 3rd or 4th decade. No obvious genetic signature that is associated with AERD.
AERD always has chronic sinus disease but not always with asthma, although it usually develops 1-5 years after onset of rhinitis. Asthma is not necessary to make dx of AERD. It needs CRS and NSAID sensitivity.
Known baseline abnormalities in AERD - decreased PGE2 is main one: https://twitter.com/MatthewBowdish/status/1087452002102083585
“All you need to know about AERD” in one slide: https://twitter.com/MatthewBowdish/status/1087452732892491776
Diagnosing AERD is difficult. History can be problematic. Small amounts of aspirin can often be tolerated, sometimes small amounts of alcohol can augment symptoms. Only way to diagnose AERD is with ASA/NSAID challenge.
83% of AERD patients will react to alcohol (nasal congestion, even wheeze). Patients with AERD appear to be sensitive to all alcohol. Mechanism is unclear.
Reactions to oral Aspirin Challenge: https://twitter.com/MatthewBowdish/status/1087454672925876224
Addition of a Leukotriene Receptor Antagonist (LTRA) does not change the outcome of oral aspirin desensitizations.
Treatment of AERD:
1. Avoid COX-1 inhibitor NSAIDs
2. Highly-selective COX-2 inhibitors and Acetaminophen are generally well-tolerated
3. ASA Desens if needed
Q: Who should get ASA Desens?
A: Pts with recurrent chronic sinusitis/polyps, all AERD pts except those well-controlled on ICS, ICS/LABA & LTMDs, those who require antiplatelet therapy w/ASA or other COX-1 inhibitors.
Optimization of ASA Desensitization: FEV1 over 60% (or 1.5 L). https://twitter.com/MatthewBowdish/status/1087458466195595264
Try to increase FEV1 at baseline. If unable, it may be OK to start since patients might have irreversible airway obstruction.
ASA Desensitization Protocol: https://twitter.com/MatthewBowdish/status/1087458962318880768
Safety of ASA Desensitization:
- Scripps have done more than 1400 challenges with only 3 systemic reactions (all responded to 1 Epi)
-Average time to reaction is 102 minutes
-Typical provoking dose is 45-100 mg ASA
Safety of asa desensitization: note expedited protocols don’t seem to be safe. Reactions can be severe. Need another blocking drug before single day desensitizations: https://twitter.com/RayFirszt/status/1087458667589296128
Cross desensitization to other NSAIDS occurs. However, you can only use ASA for desensitization purposes.
Nasal congestion improves immediately during asa desensitization. However, airway irritability remains unchanged.
Aspirin Dosing after ASA Desensitization:
-81mg ok for cardiovascular diz prevention
-325mg ok to be cross-desensitized to any doses of all NSAIDs
-650mg BID initial starting dose for AERD; about 50% can decrease to 325 mg BID after 1-6 months
https://twitter.com/RayFirszt/status/1087459807592939520
Biologics targeting TH2 inflammation seem to be effective in AERD. Biologics like omalizumab and others (anti-IL5, anti-IL4/13) may have a role in AERD but there have not been big enough studies to show that it works or helps in polyps or ASA challenges, some studies are ongoing as we speak.
“In an ideal world, it would be great to have a clinical test to confirm AERD other than desensitization.”
Salicylates are not COX inhibitors and have no effect in AERD. There is some evidence that low salicylate diet might be helpful.
Bits of Wisdom from the front lines of ASA Desensitization: https://twitter.com/MatthewBowdish/status/1087462072860893184
This is a Twitter summary from the 2019 WSAAI meeting. This summary was compiled from the tweets posted by Matthew Bowdish @MatthewBowdish and Ray Firszt @RayFirszt, who attended the 2019 Western Society of Allergy, Asthma and Immunology (WSAAI) meeting. The tweets were labeled #WSAAI. The text was edited by me.
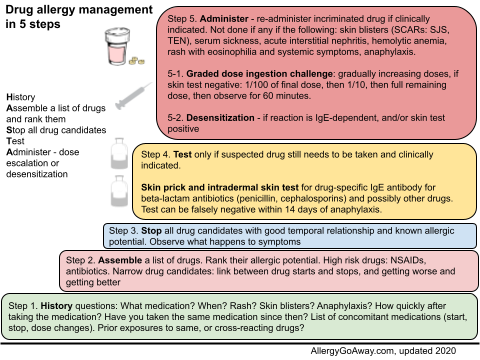
Drug allergy management in 5 steps (click to enlarge the image).
AERD is chronic eosinophilic (Type 2) inflammation of sinuses +/- the lungs with sensitivity to all COX-1 inhibiting NSAIDS with age of onset in 3rd or 4th decade. No obvious genetic signature that is associated with AERD.
AERD always has chronic sinus disease but not always with asthma, although it usually develops 1-5 years after onset of rhinitis. Asthma is not necessary to make dx of AERD. It needs CRS and NSAID sensitivity.
Known baseline abnormalities in AERD - decreased PGE2 is main one: https://twitter.com/MatthewBowdish/status/1087452002102083585
“All you need to know about AERD” in one slide: https://twitter.com/MatthewBowdish/status/1087452732892491776
Diagnosing AERD is difficult. History can be problematic. Small amounts of aspirin can often be tolerated, sometimes small amounts of alcohol can augment symptoms. Only way to diagnose AERD is with ASA/NSAID challenge.
83% of AERD patients will react to alcohol (nasal congestion, even wheeze). Patients with AERD appear to be sensitive to all alcohol. Mechanism is unclear.
Reactions to oral Aspirin Challenge: https://twitter.com/MatthewBowdish/status/1087454672925876224
Addition of a Leukotriene Receptor Antagonist (LTRA) does not change the outcome of oral aspirin desensitizations.
Treatment of AERD:
1. Avoid COX-1 inhibitor NSAIDs
2. Highly-selective COX-2 inhibitors and Acetaminophen are generally well-tolerated
3. ASA Desens if needed
Q: Who should get ASA Desens?
A: Pts with recurrent chronic sinusitis/polyps, all AERD pts except those well-controlled on ICS, ICS/LABA & LTMDs, those who require antiplatelet therapy w/ASA or other COX-1 inhibitors.
Optimization of ASA Desensitization: FEV1 over 60% (or 1.5 L). https://twitter.com/MatthewBowdish/status/1087458466195595264
Try to increase FEV1 at baseline. If unable, it may be OK to start since patients might have irreversible airway obstruction.
ASA Desensitization Protocol: https://twitter.com/MatthewBowdish/status/1087458962318880768
Safety of ASA Desensitization:
- Scripps have done more than 1400 challenges with only 3 systemic reactions (all responded to 1 Epi)
-Average time to reaction is 102 minutes
-Typical provoking dose is 45-100 mg ASA
Safety of asa desensitization: note expedited protocols don’t seem to be safe. Reactions can be severe. Need another blocking drug before single day desensitizations: https://twitter.com/RayFirszt/status/1087458667589296128
Cross desensitization to other NSAIDS occurs. However, you can only use ASA for desensitization purposes.
Nasal congestion improves immediately during asa desensitization. However, airway irritability remains unchanged.
Aspirin Dosing after ASA Desensitization:
-81mg ok for cardiovascular diz prevention
-325mg ok to be cross-desensitized to any doses of all NSAIDs
-650mg BID initial starting dose for AERD; about 50% can decrease to 325 mg BID after 1-6 months
https://twitter.com/RayFirszt/status/1087459807592939520
Biologics targeting TH2 inflammation seem to be effective in AERD. Biologics like omalizumab and others (anti-IL5, anti-IL4/13) may have a role in AERD but there have not been big enough studies to show that it works or helps in polyps or ASA challenges, some studies are ongoing as we speak.
“In an ideal world, it would be great to have a clinical test to confirm AERD other than desensitization.”
Salicylates are not COX inhibitors and have no effect in AERD. There is some evidence that low salicylate diet might be helpful.
Bits of Wisdom from the front lines of ASA Desensitization: https://twitter.com/MatthewBowdish/status/1087462072860893184
This is a Twitter summary from the 2019 WSAAI meeting. This summary was compiled from the tweets posted by Matthew Bowdish @MatthewBowdish and Ray Firszt @RayFirszt, who attended the 2019 Western Society of Allergy, Asthma and Immunology (WSAAI) meeting. The tweets were labeled #WSAAI. The text was edited by me.
Drug allergy management in 5 steps (click to enlarge the image).