Michael Schatz presented on "Asthma and Allergic Diseases During Pregnancy”.
Asthma increases risk of a number of adverse outcomes in pregnancy including preeclampsia, preterm birth, low birth weight, SGA, neonatal death, and malformations.
Potential mechs for adv outcomes in pregnant women with asthma include common pathogenesis (factors affect both asthma & reproductive fxn), confounding (smoking, race, obesity & depression), poor asthma control (hypoxia, reduced uteroplacental blood flow) & asthma meds.
SABAs - There is substantial reassuring data from large prospective and prospective trials. There are some reports of increased specific malformations w/SABAs in case-control studies, but potential confounding by asthma control/exacerbations. Benefits from SABAs outweigh possible risks.
Substantial safety data for low and medium dose ICS, but possible association with high dose ICS from retrospective database studies may be confounding by severity. ICS in pregnancy: budesonide is most studied. But there was no difference between budesonide and fluticasone, both appeared safe.
LABAs - less data than for ICS or SABA but reassuring data from retrospective cohort studies for both salmeterol and formoterol.
OCS - cohort studies have reported assoc between OCS and preeclampsia, preterm delivery, preterm birth and low birth wt, but potential confounding by severity/control/exacerbations. Conflicting data regarding association of OCS with cleft lip/palate.
Biologics:
Omalizumab: no inc risk of major congenital malforms
Mepolizumab: no evidence of fetal harm in monkeys w/30x max human dose, no human data
Reslizumab: no adv effect in animals with HDs, no human data
Benralizumab: no adv effect in animals, no human data
Dupilumab: no adv events in high doses, no human studies
Asthma Mgt Conclusions: step therapy, budesonide or fluticasone for women starting ICS in pregnancy, LABA salmeterol vs formoterol based on non-preg considerations, montelukast an alt for mild persistent asthma or add-on, tiotropium for uncontrolled on ICS/LABA.
Treatment of asthma is similar to usual treatment when pregnant. Use fluticasone or budesonide. You can still use montelukast (Singulair). Spiriva can be considered. Xolair appears OK. Regarding other biologics: continue to use them if already on them and responding.
FeNO is a good marker of asthma control in pregnancy.
MotherToBaby is a service of the non-profit Organization of Teratology Information Specialists (OTIS), a source of information on the safety of medications and other exposures during pregnancy and while breastfeeding. Patients can self register if on medications during pregnancy: https://mothertobaby.org/about-us/
Barriers to asthma control in pregnancy: smoking, clinician under-treatment, adherence, viral infections and obesity.
Allergic rhinitis
There is no data showing a direct effect of rhinitis on perinatal outcomes although snoring is associated with an increase risk of preeclampsia. Rhinitis Management Conclusions: https://twitter.com/MatthewBowdish/status/1088565184359063553
Avoid decongestants in pregnancy - no great data and some safety concerns. Pseudoephedrine would be one of choice. OK to use fluticasone, mometasone and budesonide intranasal steroids.
SPT in pregnancy can be considered. Perform in vitro sIgE, if possible, instead of SPT.
IT during pregnancy - continue if doing well, consider dose reduction.
SCIT/ Immunotherapy - Generally, do not start IT given uncertain propensity for systemic rxns, increased likelihood of systemic rxns during IT build-up, latency of effect, uncertainty of benefit. Continue immunotherapy if patient already receiving IT, pt deriving benefit, has not been prone to systemic rxns, at maintenance or effective dose and consider prophylactic dose reduction.
Epinephrine is associated with birth defects in some studies but some confounders, has the potential to reduce uteroplacental blood flow, still the drug of choice for anaphylaxis and obs suggest benefits outweigh risks. Other aspects of anaphylaxis treatment during pregnancy: https://twitter.com/MatthewBowdish/status/1088571118753968128
CU management in pregnancy: https://twitter.com/RayFirszt/status/1088566319639711744
HAE during pregnancy - use plasma derived C1inh.
Atopic dermatitis (AD) in pregnancy - topical steroids (TCS) at mild moderate potency appear safe. Some fetal growth restrictions at very high dose. There are no human data on topical calcineurin inhibitors (TCI).
Treatment of AD in pregnancy: https://twitter.com/RayFirszt/status/1088567237231792128
https://twitter.com/RayFirszt/status/1088567372166754306
This is a Twitter summary from the 2019 WSAAI meeting. This summary was compiled from the tweets posted by Matthew Bowdish @MatthewBowdish and Ray Firszt @RayFirszt, who attended the 2019 Western Society of Allergy, Asthma and Immunology (WSAAI) meeting. The tweets were labeled #WSAAI. The text was edited by me.
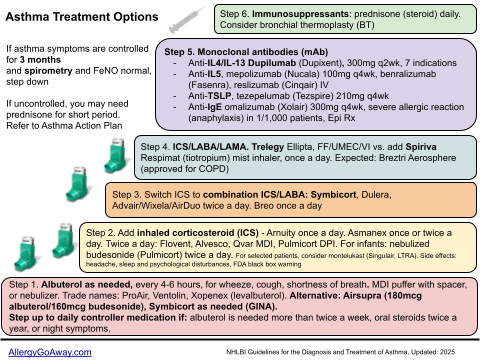
Asthma Treatment Options (click to enlarge the image).
Asthma increases risk of a number of adverse outcomes in pregnancy including preeclampsia, preterm birth, low birth weight, SGA, neonatal death, and malformations.
Potential mechs for adv outcomes in pregnant women with asthma include common pathogenesis (factors affect both asthma & reproductive fxn), confounding (smoking, race, obesity & depression), poor asthma control (hypoxia, reduced uteroplacental blood flow) & asthma meds.
SABAs - There is substantial reassuring data from large prospective and prospective trials. There are some reports of increased specific malformations w/SABAs in case-control studies, but potential confounding by asthma control/exacerbations. Benefits from SABAs outweigh possible risks.
Substantial safety data for low and medium dose ICS, but possible association with high dose ICS from retrospective database studies may be confounding by severity. ICS in pregnancy: budesonide is most studied. But there was no difference between budesonide and fluticasone, both appeared safe.
LABAs - less data than for ICS or SABA but reassuring data from retrospective cohort studies for both salmeterol and formoterol.
OCS - cohort studies have reported assoc between OCS and preeclampsia, preterm delivery, preterm birth and low birth wt, but potential confounding by severity/control/exacerbations. Conflicting data regarding association of OCS with cleft lip/palate.
Biologics:
Omalizumab: no inc risk of major congenital malforms
Mepolizumab: no evidence of fetal harm in monkeys w/30x max human dose, no human data
Reslizumab: no adv effect in animals with HDs, no human data
Benralizumab: no adv effect in animals, no human data
Dupilumab: no adv events in high doses, no human studies
Asthma Mgt Conclusions: step therapy, budesonide or fluticasone for women starting ICS in pregnancy, LABA salmeterol vs formoterol based on non-preg considerations, montelukast an alt for mild persistent asthma or add-on, tiotropium for uncontrolled on ICS/LABA.
Treatment of asthma is similar to usual treatment when pregnant. Use fluticasone or budesonide. You can still use montelukast (Singulair). Spiriva can be considered. Xolair appears OK. Regarding other biologics: continue to use them if already on them and responding.
FeNO is a good marker of asthma control in pregnancy.
MotherToBaby is a service of the non-profit Organization of Teratology Information Specialists (OTIS), a source of information on the safety of medications and other exposures during pregnancy and while breastfeeding. Patients can self register if on medications during pregnancy: https://mothertobaby.org/about-us/
Barriers to asthma control in pregnancy: smoking, clinician under-treatment, adherence, viral infections and obesity.
Allergic rhinitis
There is no data showing a direct effect of rhinitis on perinatal outcomes although snoring is associated with an increase risk of preeclampsia. Rhinitis Management Conclusions: https://twitter.com/MatthewBowdish/status/1088565184359063553
Avoid decongestants in pregnancy - no great data and some safety concerns. Pseudoephedrine would be one of choice. OK to use fluticasone, mometasone and budesonide intranasal steroids.
SPT in pregnancy can be considered. Perform in vitro sIgE, if possible, instead of SPT.
IT during pregnancy - continue if doing well, consider dose reduction.
SCIT/ Immunotherapy - Generally, do not start IT given uncertain propensity for systemic rxns, increased likelihood of systemic rxns during IT build-up, latency of effect, uncertainty of benefit. Continue immunotherapy if patient already receiving IT, pt deriving benefit, has not been prone to systemic rxns, at maintenance or effective dose and consider prophylactic dose reduction.
Epinephrine is associated with birth defects in some studies but some confounders, has the potential to reduce uteroplacental blood flow, still the drug of choice for anaphylaxis and obs suggest benefits outweigh risks. Other aspects of anaphylaxis treatment during pregnancy: https://twitter.com/MatthewBowdish/status/1088571118753968128
CU management in pregnancy: https://twitter.com/RayFirszt/status/1088566319639711744
HAE during pregnancy - use plasma derived C1inh.
Atopic dermatitis (AD) in pregnancy - topical steroids (TCS) at mild moderate potency appear safe. Some fetal growth restrictions at very high dose. There are no human data on topical calcineurin inhibitors (TCI).
Treatment of AD in pregnancy: https://twitter.com/RayFirszt/status/1088567237231792128
https://twitter.com/RayFirszt/status/1088567372166754306
This is a Twitter summary from the 2019 WSAAI meeting. This summary was compiled from the tweets posted by Matthew Bowdish @MatthewBowdish and Ray Firszt @RayFirszt, who attended the 2019 Western Society of Allergy, Asthma and Immunology (WSAAI) meeting. The tweets were labeled #WSAAI. The text was edited by me.
Asthma Treatment Options (click to enlarge the image).