 Lung function testing changed the assessment in 11% of pediatric patients with asthma - the disease status was worse than expected. However, spirometry should not be seen as the "gold standard" for assessing asthma control. Instead, a combination of objective and subjective measures provides the best approach.
Lung function testing changed the assessment in 11% of pediatric patients with asthma - the disease status was worse than expected. However, spirometry should not be seen as the "gold standard" for assessing asthma control. Instead, a combination of objective and subjective measures provides the best approach.In study presented at the 2010 ACAAI Annual Meeting, the initial analysis, excluding spirometry, showed that participants had well-controlled asthma 67% of visits. However, when spirometry was included, 11% of the patients were reclassified to have uncontrolled asthma.
William Dolen, MD comments: "All people who do the subjective assessment and also do spirometry have patients who give you an excellent control score and yet when you do the spirometry, it's terrible. It can also work the other way -- patients complain about symptoms, but have excellent lung function on spirometry. Monitoring lung function by spirometry is key to the successful control of asthma in more severe patients. But lung function testing is not done as often as it should be because many asthma patients are treated by their family doctor. They don't have spirometers and they're not trained in how to interpret the results, so the testing is not done."
Most board-certified allergists have spirometers in their clinics and can provide an accurate assessment of your asthma control within minutes. The youngest age to perform spirometry with reproducible results varies between 5 and 7 years, depending on the patient.
William Dolen, MD comments: "All people who do the subjective assessment and also do spirometry have patients who give you an excellent control score and yet when you do the spirometry, it's terrible. It can also work the other way -- patients complain about symptoms, but have excellent lung function on spirometry. Monitoring lung function by spirometry is key to the successful control of asthma in more severe patients. But lung function testing is not done as often as it should be because many asthma patients are treated by their family doctor. They don't have spirometers and they're not trained in how to interpret the results, so the testing is not done."
Most board-certified allergists have spirometers in their clinics and can provide an accurate assessment of your asthma control within minutes. The youngest age to perform spirometry with reproducible results varies between 5 and 7 years, depending on the patient.
References:
ACAAI: Lung Tests Help Assess Asthma in Young Patients. MedPage Today.
Impulse oscillometry for evaluation pediatric asthma - noninvasive rapid technique requiring only passive cooperation http://goo.gl/znFYg
Daily home spirometry does not reduce exacerbations in children with severe asthma. ERJ, 2012.
Daily home spirometry does not reduce exacerbations in children with severe asthma. ERJ, 2012.
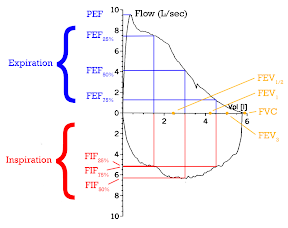
Image source: Spirometry, from Wikipedia, the free encyclopedia, GNU Free Documentation License.
PFTs: Question everything http://bit.ly/1j7WYTz