 The Journal of Allergy and Clinical Immunology recently published the updated guidelines for diagnosis and management of allergic and non-allergic rhinitis. Some of the recommendations are summarized below.
The Journal of Allergy and Clinical Immunology recently published the updated guidelines for diagnosis and management of allergic and non-allergic rhinitis. Some of the recommendations are summarized below.The prevalence of AR is 10-30% in adults and up to 40% in children.
Comorbidities of allergic rhinitis (AR): asthma, sinusitis, and obstructive sleep apnea (OSA). The comorbidities may require evaluation with PFTs for asthma or a sleep study for OSA. Sleepiness and sleep-disordered breathing may be found in 19-29% of children with positive allergy test (http://goo.gl/AfCWZ).
Emerging diagnostic procedure: acoustic rhinometry.
Emerging therapeutic procedure: radiofrequency volumetric tissue reduction.
The term "episodic rhinitis" is introduced to describe AR caused by sporadic exposures to inhalant aeroallergens
Oral decongestants should be avoided in children younger than 6 years of age.

Medications for Allergic Rhinitis. See more Mind Maps of Allergic Rhinitis.
Oral antihistamines
Oral antihistamines are less effective for nasal congestion and INS are generally preferred for more severe AR.
Oral antihistamines are less effective than INS. However, they are similarly effective to INS for ocular symptoms in AR/AC.
Oral antihistamines are effective in reducing rhinorrhea, sneezing, and itching but have little effect on nasal congestion (this is where INS play the major role).
Oral antihistamines are ineffective for non-AR. They can achieve adequate control of moderate AR but INS are usually needed for severe AR.
Second-generation oral antihistamines fexofenadine, loratadine, and desloratadine do not cause sedation at recommended doses.
Second-generation antihistamines considered as safe agents during pregnancy (Zyrtec is pregnancy category B).
Intranasal antihistamines
Intranasal antihistamines have a rapid onset of action (3-4 hours) which makes them suitable for RRN use in episodic AR.
Intranasal antihistamines are better than oral antihistamines for nasal congestion but yet not as effective as INS.
Intranasal antihistamines are also approved for vasomotor rhinitis (non-AR) which makes them a good option for patients with mixed rhinitis (AR/non-AR).
Patients often complain of bitter taste with intranasal azelastine but the newer intranasal olopatadine (Patanase) is better tolerated.
Intranasal steroids (INS)
INS are the most effective therapy for AR
PRN use of INS may be effective for seasonal and episodic AR. New from the guidelines: intranasal corticosteroids (INS) are recommended for PRN use.
Typical onset of action of INS is within 12 hours which is slower than with oral or intranasal antihistamines (3-4 hours).
However, some patients report effect from INS within 3-h hourse (similar to antihistamines), hence the recommendation for PRN use.
INS are more effective than combination therapy with oral antihistamine and LTRA.
For ocular symptoms of AR, efficacy of INS is similar to that of oral antihistamines. INS may be used for symptoms of allergic conjunctivitis associated with rhinitis.
INS can be used for mixed rhinitis (AR and non-AR) -- similar to intranasal antihistamines.
INS do not cause growth suppression in children
Systemic Steroids
Oral steroids may be used for very severe nasal symptoms when given as a short course (5 - 7 days). Single or repeated administration of intramuscular steroids should be discouraged.
Leukotrienes (LTRA)
LTRA have not been shown to be more efficacious than oral antihistamines for AR.
LTRA are approved for both AR and asthma and may be a good treatment option for patients who have both conditions.
Intranasal anticholinergic
Intranasal anticholinergic (ipratropium) has a rapid onset of action (3-4 hours, similar to intranasal antihistamines) and can be used for for episodic rhinitis.
Ipratropium reduces rhinorrhea but is otherwise ineffective for congestion and other symptoms of AR.
Intranasal cromolyn
Intranasal cromolyn can be used for maintenance treatment of AR.
Onset of action is very slow (4-7 days) and the full benefit may not be evident for weeks.
Intranasal cromolyn is not as effective as INS.
References:
Guidelines Updated for Diagnosis and Treatment of Rhinitis. Laurie Barclay. Medscape.
The Diagnosis and Management of Rhinitis: An Updated Practice Parameter. The Journal of Allergy and Clinical Immunology, Volume 122, Issue 2, Supplement (August 2008).
Image source: Wikipedia, a Creative Commons license.
Allergic Rhinitis: A Short Review
Mind Maps: Allergic Rhinitis
Japanese guideline for allergic rhinitis: An evidence-based step-by-step strategy for treatment is described. Allergol Int. 2011 Mar;60(2):171-89.
Nasal carbon dioxide is a potentially efficacious treatment for the symptoms of allergic rhinitis http://goo.gl/oNw56
Nonallergic rhinitis, CCJM 2012 review.
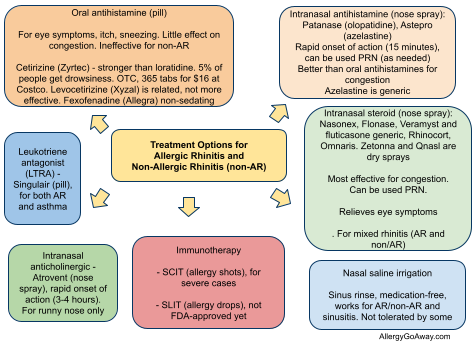
Treatment Options for Allergic Rhinitis (click to enlarge the image).
Nonallergic rhinitis, CCJM 2012 review.
Treatment Options for Allergic Rhinitis (click to enlarge the image).