 -------------
-------------Patient perceptions regarding local reactions from allergen immunotherapy injections: Not a Big Deal.
Annals of Allergy, Asthma and Immunology, 2008, vol. 101, no. 1, pp. 96 - 100.
Local reactions to immunotherapy are not predictive of future systemic reactions. Seventy-one percent of 249 patients undergoing immunotherapy completed a survey. Of those patients who reported local reactions, 84.7% reported local reactions smaller than the palm of the hand and 81.9% deemed local reactions not to be bothersome at all or only slightly bothersome. Of those who experienced local reactions, 96.0% stated they would not stop immunotherapy because of these local reactions.
-------------
Bronchodilator efficacy of indacaterol, a novel once-daily 2-agonist, in patients with persistent asthma: Works Fast and for 24 Hours.
Annals of Allergy, Asthma and Immunology, 2008, vol. 101, no. 1, pp. 90 - 95.
Indacaterol is a novel once-daily inhaled 2-agonist in development for the treatment of asthma or COPD. In 25 patients, indacaterol demonstrates sustained bronchodilator efficacy throughout the full 24-hour period, with a rapid onset of action and a good safety profile.
-------------
The effects of the nasal antihistamines olopatadine and azelastine in nasal allergen provocation: Both Worked Well.
Annals of Allergy, Asthma and Immunology, 2008, vol. 101, no. 1, pp. 82 - 89.
Olopatadine, an antihistamine used in allergic conjunctivitis, is under development as a nasal preparation for the treatment of allergic rhinitis. In 20 asymptomatic subjects with seasonal allergic rhinitis, olopatadine, 0.1%, inhibited lysozyme levels, but olopatadine, 0.2%, inhibited histamine, albumin, and lysozyme. The effects of olopatadine, 0.1%, were comparable to those of azelastine, 0.1%.
Patanase was approved by the FDA in April, 2008.
-------------
Intranasally administered corticosteroids and neuropsychiatric disturbances: a review of the International Pharmacovigilance Programme of the World Health Organization: There is a Probable Connection.
Annals of Allergy, Asthma and Immunology, 2008, vol. 101, no. 1, pp. 67 - 73.
Systemic use of corticosteroids is connected with a variety of psychiatric and neurologic effects. Intranasal steroids are considered to exert minimal systemic effects. An unexpected cluster of case reports of neuropsychiatric disorders during intranasal corticosteroid use was reported to the WHO: 429 reports were received from 16 countries (1980-April 2006). Events included nervousness, anxiety, agitation, insomnia, emotional lability, depression, somnolence, confusion, convulsions, and migraine. In 97 of 108 patients who had discontinued use of the intranasal corticosteroid, the reaction abated. Of 41 patients, 32 had a relapse when the drug was reintroduced.
-------------
Economic burden of rhinitis in managed care: a retrospective claims data analysis: $ 657 per patient each year.
Annals of Allergy, Asthma and Immunology, 2008, vol. 101, no. 1, pp. 23 - 29.
Average rhinitis-related total costs were $ 657 per patient each year ($ 319 in medical costs and $ 338 in pharmacy costs). Antihistamines were the most common rhinitis medication, followed by intranasal corticosteroids (INSs) and montelukast.
-------------
Omalizumab and Churg-Strauss syndrome: 3 Cases.
JACI, Volume 122, Issue 1, Page 217 (July 2008).
One can use omalizumab in patients with CSS to treat and control asthma, but it was also demonstrated that anti-IgE does not control CSS activity. Systemic corticosteroids are the drug of choice to treat CSS, and its tapering in asthmatic patients has to be made with caution, especially when CSS is suspected.
-------------
The use of serum-specific IgE measurements for the diagnosis of peanut, tree nut, and seed allergy: A Valuable Tool.
JACI, Volume 122, Issue 1, Pages 145-151 (July 2008).
The gold standard for diagnosing food allergy is the double-blind, placebo-controlled food challenge. Diagnostic food-specific IgE levels might help circumvent the need for food challenges. Quantification of food-specific IgE is a valuable tool that will aid in the diagnosis of symptomatic food allergy and might decrease the need for double-blind, placebo-controlled food challenges.
-------------
Use of multiple doses of epinephrine in food-induced anaphylaxis in children: Required in 19%.
JACI, Volume 122, Issue 1, Pages 133-138 (July 2008).
Food allergy is the most common cause of anaphylaxis outside the hospital setting. In a survey of 78 children, 19% of food-induced anaphylactic reactions were treated with more than 1 dose of epinephrine. Patients receiving multiple doses of epinephrine more often had asthma.
-------------
Sublingual immunotherapy for large local reactions caused by honeybee sting: A double-blind, placebo-controlled trial: A Viable Alternative.
JACI, Volume 122, Issue 1, Pages 44-48 (July 2008).
According to the Italian authors, sublingual immunotherapy (SLIT) proved effective and safe in respiratory allergy. Honeybee SLIT significantly reduced the extent of large local reactions (LLRs), and its safety profile was good.
-------------
A time efficient way to stay up-to-date with medical literature
"How do you eat in elephant? In small bites." The same rule probably applies to staying current with the ever expanding avalanche of medical literature. One can try the following approach:
1. Subscribe to the RSS feeds of the 5 major medical journals (NEJM, JAMA, BMJ, Lancet and Annals) plus 2-3 subpecialty journals in your field of interest.
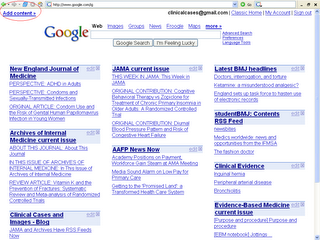
Medical Journals tab: A screenshot of iGoogle with RSS feeds from the major medical journals.
2. Read the journal on the day it is published online, for example, NEJM on Wednesdays.
3. Use text-to-speech to listen to the articles you do not have time to read.
4. Listen to journal podcasts. Click here to subscribe the podcasts of the 4 major journals in iGoogle.
Related:
Make Your Own "Medical Journal" with iGoogle Personalized Page
Share iGoogle Tabs with Medical Journals, Podcasts and Gadgets
Annals of Internal Medicine Launches Podcast and Audio Summaries
Text-to-Speech Programs and Continuous Medical Education
Image source: OpenClipArt, public domain.